Antimicrobial Resistance: A Threat to Neglected Tropical Disease Elimination
One Health Newsletter: Volume 17, Issue 1
Introduction
he fight against antimicrobial resistance (AMR) is one of the four major priorities in the implementation of the One Health strategies, as outlined by international health agencies, where other major priorities include zoonoses, emerging diseases, and food safety. Neglected tropical diseases (NTDs) represent a group of parasitic, viral, fungal, bacterial, and protozoan infections that primarily affect impoverished communities in tropical climates. These diseases have been labeled "neglected" because they predominantly affect developing countries and, until recent years, were not prioritized by the global health agenda (World Health Organization, 2024). In 2015, the global community prioritized eliminating NTDs by the year 2030, as detailed in the Sustainable Development Goals that were adopted by members of the United Nations (UN). The World Health Organization (WHO) and partner nations have made significant strides toward achieving this feat, with 47 countries reporting having successfully eliminated at least one NTD, as of December 2022 (Akinsolu et al., 2019). However, the rise of AMR threatens global progress toward NTD eradication.
AMR describes the adaptation of pathogen agents to evolve in such a way that conventional drug therapies are no longer sufficient treatments against them (WHO, 2023). NTDs are at increased risk of developing resistance due to a limited variety of drugs available in low- and middle-income countries (LMIC) and a lack of alternative treatment measures. As recent research indicates that six major NTDs have displayed drug resistance, AMR research must be prioritized and incentivized by the global community to mitigate this looming threat (Akinsolu et al., 2019).

Image from the U.S. Center's for Disease Control and Prevention's Public Health Image Library.
Literature Review
The WHO has identified 20 different NTDs, 11 of which are considered major NTDs, including Chagas disease, food-borne trematodiasis, human African trypanosomiasis (HAT), leishmaniasis, leprosy, lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminths (STH), taeniasis, and trachoma (Fig. 1) (Akinsolu et al., 2019; Kondovych, 2021).
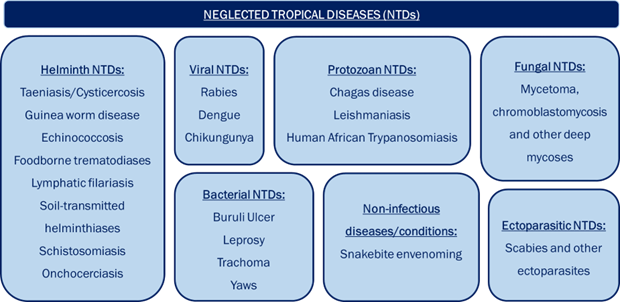
Figure 1: Neglected tropical diseases by category, according to the World Health Organization’s classification. Reprinted From “World Neglected Tropical Diseases Day 2021” by S. Kondovych, 2021, Life Chemicals Blog.
NTD control is challenging due to the pathogen's complex life and transmission cycles, attributing to significant social, economic, and health disparities. NTDs affect over one billion people globally, or approximately one-sixth of the world’s population, and are more abundant in areas with limited access to clean water, sanitation, and reliable healthcare (WHO, 2024). These diseases thrive in rural areas, conflict zones, and other difficult-to-reach regions, with 10 global hotspots for NTDs, with the highest burden in Sub-Saharan Africa (Fig. 2) (Hotez, 2014).
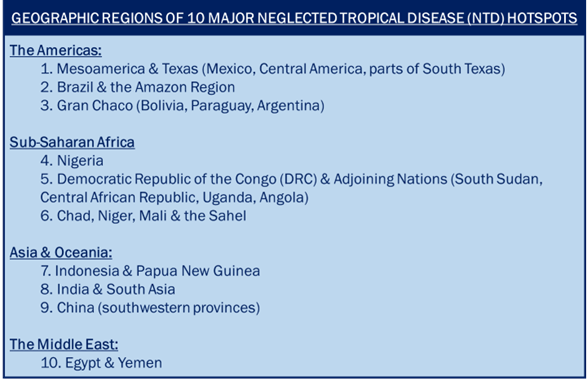
Figure 2: Ten global NTD hotspots categorized by geographic region. Adapted from Hotez (2014).
Antimicrobial Resistance. The term "antimicrobial" refers to any treatment type - antibiotic, antiviral, antifungal, and antiparasitic – that kills or inhibits the growth of pathogens, such as the causative agents of NTDs (WHO, 2023). These organisms have evolved to evade conventional drug therapies, and AMR is particularly alarming as elimination strategies and the existing therapeutic arsenal are extremely limited (Akinsolu et al., 2019). The WHO has reported AMR for several classes of NTD drugs, namely kinetoplastids, used to treat human African trypanosomiasis, and most medicines used in the treatment of leprosy (WHO, 2023). Overall, the risk for developing drug resistance is highest for helminths, including intestinal nematodes (soil-transmitted helminthiases), followed by filariae (onchocerciasis and lymphatic filariasis) and trematodes (schistosomiasis). Authors of one research study determined that six of the 11 major NTDs – human African trypanosomiasis, leishmaniasis, onchocerciasis, schistosomiasis, soil-transmitted helminths, and trachoma – have conferred resistance to traditional drug therapies (Akinsolu et al., 2019).
One common elimination strategy for NTDs is mass drug administration (MDA), which broadly and routinely targets at-risk populations to be treated for NTDs without the need for individual diagnosis, as recommended by the WHO (Akinsolu et al., 2019). Broad-sweeping NTD campaigns, while necessary, are not sustainable because the drug arsenals for these conditions are either limited or waning in effectiveness. This practice also poses heightened risks for diseases where there is sole reliance on one existing treatment, like schistosomiasis (Walker et al., 2021). Many drugs currently in use for the treatment of NTDs are becoming increasingly ineffective due to climbing rates of resistance, highlighting the dual threat of AMR and NTDs (Akinsolu et al., 2019).
To combat the rising threat of AMR and preserve progress toward the UN Sustainable Development Goals, continued new drug development is essential. However, there are many deterrents and few incentives associated with novel drug development, particularly for NTDs. The financial return on NTD investments is low, given that the populations of greatest need are in areas of extreme poverty (Akinsolu et al., 2019).
Discussion
To overcome the combination of high costs and little financial gain that dissuades pharmaceutical companies from antibiotic research and development (R&D), economic incentives must be implemented through a blend of "push" and "pull" incentives (Årdal et al., 2018). According to Årdal et al. (2018), push incentives describe initiatives that support R&D directly, including grants, tax credits or extensions, and public/private partnerships for drug development. Pull incentives describe mechanisms that reward successful R&D outcomes, such as market entry rewards, market exclusivity extensions, reimbursements, and purchase guarantees, once the drug is approved. These approaches should be implemented simultaneously, allowing companies to eliminate financial risk.
Financial incentives in the form of tax credits compensate for the high costs of antibiotic production, motivating companies to explore novel approaches under lower-risk conditions (Årdal et al., 2018). In addition to tax credits, a market entry reward (MER), or a financially valuable prize given to a manufacturer when their qualifying drug enters the market, would also invigorate antimicrobial drug production. The Driving Reinvestment in R&D and Responsible Antibiotic Use (DRIVE-AB) project has projected that "a market entry reward of one billion dollars per antibiotic globally could quadruple the number of new antibiotics coming to the market in the next 30 years" (Årdal et al., p.6, 2018). These efforts should be pursued by all capable governments, as such an infusion of new and effective antimicrobial treatments would reinvigorate a myriad of global disease mitigation and elimination efforts, including the battle against NTDs.
Additionally, other specialized programs exist to increase incentives for companies to engage in NTD-focused drug development. For example, the U.S. Food and Drug Administration (FDA) has established a priority review voucher program for NTD drug applications, recognizing that there has been limited progress in recent decades in the development of drugs and vaccines for NTDs (U.S. FDA, 2016). The FDA asserts that because these diseases are found primarily in impoverished and developing nations, existing incentives have not adequately encouraged development, a precedent this legislation aims to address. This program expedites the R&D process, saving companies time and money without offering a lump sum. The European Medicines Agency (EMA) has launched similar incentives for diseases of significant interest to public health (like NTDs) (EMA, 2023).
Conclusion
The UN Sustainable Development Goals highlight the elimination of NTDs as a key global health priority to be achieved by the year 2030, and yet, the rise of AMR obstructs progress toward this goal. To counter this threat and address health priorities in a myriad of categories, the global health community must focus all necessary efforts on incentivizing a period of rapid innovation for antimicrobial drug development. The FDA and equivalent global regulatory agencies must allocate fiscal resources for economic incentives to replenish the waning pipeline of effective antimicrobial drugs, monitor and manage the increasing threat of NTD drug resistance, and pursue progress toward NTD elimination worldwide.
References
Akinsolu, F. T., Nemieboka, P. O., Njuguna, D. W., Ahadji, M. N., Dezső, D., and Varga, O. (2019). Emerging resistance of neglected tropical diseases: A scoping review of the literature. International Journal of Environmental Research and Public Health, 16(11), Article e1925. https://doi.org/10.3390/ijerph16111925
Årdal, C., Findlay, D., Savic, M., Carmeli, Y., Gyssens, I., Laxminarayan, R., Outterson, K., and Rex, J. H. (2018). Revitalizing the antibiotic pipeline: Stimulating innovation while driving sustainable use and global access [Executive summary]. Innovative Medicines Initiative. https://www.ihi.europa.eu/sites/default/files/projects/documents/DRIVE-AB-Executive-Summary-Jan2018.pdf
European Medicines Agency. (2023). Article 58 application. https://www.ema.europa.eu/en/glossary/article-58-application
Hotez, P. J. (2014). Ten global "hotspots" for the neglected tropical diseases. PLoS Neglected Tropical Diseases, 8(5), Article e2496. https://doi.org/10.1371/journal.pntd.0002496
Kondovych, S. (2021). World Neglected Tropical Diseases Day 2021. Life Chemicals Blog. https://lifechemicals.com/blog/computational-chemistry/346-world-neglected-tropical-diseases-day-2021
U.S. Food and Drug Administration. (2016). Tropical disease priority review vouchers: Guidance for industry. https://www.fda.gov/media/72569/download
Walker, M., Hamley, J. I. D., Milton, P., Monnot, F., Kinrade, S., Specht, S., Pedrique, B., and Basáñez, M. G. (2021). Supporting drug development for neglected tropical diseases using mathematical modeling. Clinical Infectious Diseases, 73 (6): e1391-e1396. https://doi.org/10.1093/cid/ciab350
World Health Organization. (2023). Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
World Health Organization. (2024). Neglected tropical diseases. https://www.who.int/news-room/questions-and-answers/item/neglected-tropical-diseases
More Articles in this Issue