One Health Newsletter
Zoonoses in Ethiopia
Author
Rebecca Laes-Kushner
One Health programs use an interdisciplinary approach to tackle the transmission of diseases between humans and animals, known as zoonotic diseases, by bringing together physicians, veterinarians, epidemiologists, and other experts to track, contain, and treat zoonoses. Approximately 60% of emerging infectious diseases are zoonoses, most of which originate in wildlife.1 Humans are at-risk for zoonotic disease transmission when they come into direct or indirect contact with contaminated food, water, bodily fluids from infected animals, or surfaces diseased animals have touched. In Ethiopia, zoonoses are often transmitted to small-scale farmers whose domestic livestock have become infected after sharing pasture or water with diseased wildlife.
One Health in Ethiopia
For Dr. Mohammed Ibrahim, assistant professor of epidemiology at Jigjiga University in Ethiopia, his mission is to prevent the spread of zoonoses. Trained at the Swiss Tropical and Public Health Institute (SwissTPH) and the University of Basel in Switzerland, Dr. Ibrahim uses a One Health approach, collaborating with medical, veterinary, and environmental experts to track and combat zoonoses. Dr. Ibrahim and his colleagues at Jigjiga University's College of Veterinary Medicine tackle diseases such as rabies, anthrax, brucellosis, Q fever, and Lumpy Skin Disease (Table 1).
|
Disease |
Transmission Route Clinical Signs and Symptoms |
||
|
Brucellosis |
Transmission Route: Unpasteurized dairy products, raw/undercooked meat Clinical Signs and Symptoms: Abortions, birth of weak calves |
||
|
Rabies |
Transmission Route: Saliva Clinical Signs and Symptoms: Behavior change (more aggressive or depressed), erection in males, noises due to vocal cord spasms, weakness in hindquarters |
||
|
Anthrax |
Transmission Route: Ingestion of spores, which can remain viable in soil for years after diseased animal carcass decomposes Clinical Signs and Symptoms: Sudden death |
||
|
Leptospirosis |
Transmission Route: Contact with infected urine or aborted fetuses Clinical Signs and Symptoms: Infertility, abortion in cows, reduction in milk |
||
|
Echinococcosis |
Transmission Route: Dogs ingest infected meat and defecate in fields where livestock ingest eggs Clinical Signs and Symptoms: Cysts with larvae inside animal’s organs |
||
|
Q fever |
Transmission Route: Contact with infected fluids, afterbirth Clinical Signs and Symptoms: Abortions, stillbirths |
||
|
Salmonellosis |
Transmission Route: Manure Clinical Signs and Symptoms: Diarrhea, joint infections, death |
||
|
Bovine tuberculosis |
Transmission Route: Aerosol from coughing, urine, food and water Clinical Signs and Symptoms: Cough, pneumonia, death |
||
|
Helminthiasis |
Transmission Route: Eggs in feces or urine that contaminate water or soil; exacerbated by poor sanitation/lack of clean drinking water Clinical Signs and Symptoms: Reduction in food intake, poor weight gain, death |
||
|
Schistosomiasis |
Transmission Route: Freshwater snails release larvae that penetrate the skin during contact with the water; sick people then spread eggs through defecation/urination, contaminating new water sources; exacerbated by poor sanitation/lack of clean drinking water Clinical Signs and Symptoms: Weight loss, organ damage |
Table 1. Major zoonotic diseases in Ethiopia and principal characteristics (Sources: U.S. Centers for Disease Control and Prevention, 2020; European Centre for Disease Prevention and Control, 2020; World Organisation for Animal Health, 2020; CABI, 2020).
Somali State in Ethiopia
Figure 1. Map of Ethiopia, including Somalia State. (Sources: Horn of Africa from Central Intelligence Agency, 2020; Somali State from Golbez “maps/Ethiopia”, licensed under CC 2.5 Generic license; compilation licensed under CC 2.5 by Rebecca Laes-Kushner)
Dr. Ibrahim works in the Somali Region of Ethiopia (Figure 1), which is home to nomadic pastoralists and lacks the infrastructure (roads, electricity, availability of medicine) found elsewhere in Ethiopia. Dr. Ibrahim educates Somali pastoralists about zoonoses and tracks diseases in their livestock. Research by Dr. Ibrahim and his Swiss and Ethiopian associates found rates of Rift Valley Fever (RVF) seroprevalence in camels (42.6%) and cattle (17.9%), with rates between 6% and 13% for humans, goats, and sheep.6 The researchers also found seroprevalence of Q fever in 26.3% of humans, 28.9% of sheep, and about half of the camels (55.7%) and goats (48.8%) in the region. Q fever is usually transmitted due to the traditional practice of consuming raw milk.6 People with Q fever can develop pneumonia and acute respiratory distress syndrome (ARDS), which has a 30% - 45% mortality rate.7
Livestock in Ethiopia
With over 62 million cattle, according to the Food and Agriculture Organization of the United Nations (2020), Ethiopia has the highest livestock population in Africa and the fifth-highest in the world, making control of zoonotic diseases critical (Table 2).8 Agricultural households own an average of 3.3 cattle apiece and have livestock assets of US $720.9,10
|
Country # Heads of Cattle* |
Human Tuberculosis rate** |
|
|
Brazil 213,523,056 |
45 |
|
|
India 184,464,035 |
199 |
|
|
USA 94,298,000 |
3 |
|
|
China 63,271,250 |
61 |
|
|
Ethiopia 62,599,736 |
151 |
|
|
Argentina 53,928,990 |
27 |
|
|
Pakistan 46,084,000 |
265 |
|
|
Mexico 34,820,271 |
23 |
|
|
Sudan 31,223,000 |
71 |
|
|
Chad 29,063,152 |
142 |
|
|
Tanzania 27,427,658 |
253 |
|
|
Australia 26,395,734 |
7 |
|
|
Colombia 25,557,340 |
33 |
|
|
Bangladesh 24,086,000 |
221 |
|
|
Nigeria 21,418,189 |
219 |
|
Table 2. Livestock inventory and human tuberculosis rates (Sources: *Food and Agriculture Organization of the United Nations, 2020; **World Health Organization, 2020).
Tuberculosis in Ethiopia
The two main tuberculosis (TB) strains are Mycobacterium tuberculosis (mTB) in humans and Mycobacterium bovis in cattle (Bovine tuberculosis, bTB), although both strains can jump to the other species. Ethiopia has one of the highest human TB rates at 151 per 100,000 (Table 2), compared with 28 per 100,000 in Europe and 3 per 100,000 in the US.11,12 Moreover, because bTB is resistant to pyrazinamide, one of the main antibiotics used to treat TB, physicians caring for human patients may provide ineffective treatment if they do not know that the person has bTB and not mTB.
Studies have found a higher prevalence of TB among cattle owned by farmers who have TB themselves. Meanwhile, proximity to their animals and drinking raw milk are associated with higher TB rates among farmers.13,14 Both mTB and bTB have been identified in owners and milk from cows infected with TB. Epidemiologists and veterinarians in Ethiopia use the rapid intradermal tuberculin skin test (TST) on cattle, where animals are injected with tuberculin, and then 72 hours later, those whose skin has thickened at least 4 mm are considered tubercular.
The Economic Impact of Tuberculosis
In developed countries, farmers often receive governmental or insurance compensation when diseased animals or whole herds are destroyed, but such financial reparation is extremely rare in Ethiopia. Dr. Ibrahim estimates a single cow costs at least US $130 and says farmers are often reluctant to cull diseased animals. Households purchase cattle for farm use, such as plowing, and as insurance for future financial needs. For small farmers in a country with a per capita income of US $790 in 2018, the loss of even one animal has a substantial impact on the family's income. “It is life or death for the owner; it is their livelihood,” Dr. Ibrahim says.15
Although the majority of farmers own only a handful of cattle, the region around Addis Ababa, the capital of Ethiopia, is home to commercial dairy farms with exotic animals—exotic, that is, to Africa. Holstein-Fresian cows are bred because they produce significantly more milk and for more extended periods than the native Zebu cattle (Figure 2). Unfortunately, Holsteins are more likely to have TB than Zebu cattle (Odds Ratio = 2 - 15)16, 17, 18, and studies have shown that while 3% - 5% of cattle in small pastoral households have bTB, large dairy herds in urban regions can have a prevalence rate of over 50%.14, 19, 20
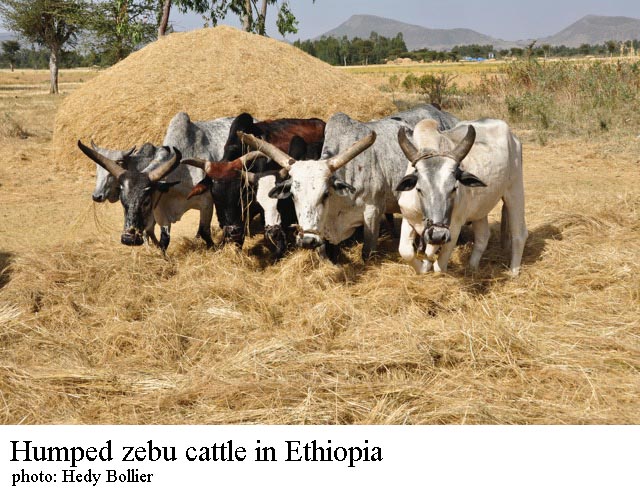
Figure 2. Native Zebu cattle in Ethiopia. (Source: Hedy Bollier)
Improving Systems in Ethiopia
Tackling bTB is the focus of the Ethiopia Control of Bovine Tuberculosis Strategies’ (ETHICOBOTS) five-year research project, which brings together epidemiologists, veterinarians, and medical experts, as well as social scientists who study the culture of farmers and their interactions with their animals. ETHICOBOTS analyzes disease control strategies, including cattle vaccination, to determine efficacy, cost-efficiency, and acceptance by farmers. Dr. Ibrahim feels solutions are needed “that will be good both at the public and family levels.” His priorities are:
- Establishment of good diagnostic centers that collect samples and report on incidence rates
- A robust countrywide disease surveillance system
- Infrastructure in pastoral regions that lack adequate roads, internet, and reliable electricity
- A better drug supply for veterinarians who often lack medication to treat sick animals
Dr. Ibrahim believes that insurance programs can be developed after surveillance infrastructures are better developed. Meanwhile, Dr. Ibrahim will continue to monitor zoonotic diseases in the Somali state and educate farmers about disease risk and transmission.
References
- Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990-993.
- US Centers for Disease Control and Prevention. Diseases and Conditions. 2020. https://www.cdc.gov/. Accessed May 20, 2020.
- European Centre for Disease Prevention and Control. Infectious disease. 2020. https://www.ecdc.europa.eu/en. Accessed May 28, 2020.
- World Organisation for Animal Health. Animal health in the world. 2020. https://www.oie.int/. Accessed May 27, 2020.
- Invasive Species Compendium. Wallingford, UK: CAB International; 2020. www.cabi.org/isc. Accessed May 27, 2020.
- Ibrahim M, Schelling E, Zinsstag J, Hattendorf J, Andargie E, Tschopp R. Sero-prevalence of brucellosis, Q-fever and Rift Valley Fever in humans and livestock in Somali region, Ethiopia. bioRxiv. 2020; 928374.
- Matthay MA, Zemans RL, Zimmerman GA, et al. Acute respiratory distress syndrome. Nature Reviews Disease Primers. 2019;5(1).
- Food and Agriculture Organization of the United Nations. Live animals [Data set]. 2020. http://www.fao.org/faostat/en/#data/QA
- Ethiopian Central Statistical Agency. Key findings of the 2017-2018 (2010 E.C.) agricultural sample surveys. http://www.csa.gov.et/ehioinfo-internal?download=915:key-findings-of-the-2017-2018-agricultural-sample-surveys
- Bachewe FN, Minten B, Tadesse F, Taffesse AS. The evolving livestock sector in Ethiopia: Growth by heads, not by productivity. 2018. https://www.ifpri.org/publication/evolving-livestock-sector-ethiopia-growth-heads-not-productivity. Accessed May 15, 2020.
- World Health Organization. Incidence: data by WHO region [Data set]. Global Health Observatory data repository. https://apps.who.int/gho/data/view.main.57036ALL?lang=en.
- World Health Organization. Tuberculosis (TB): Tuberculosis country profile. 2020. https://www.who.int/tb/country/data/profiles/en/
- Mohamed A. Bovine tuberculosis at the human–livestock–wildlife interface and its control through one health approach in the Ethiopian Somali Pastoralists: A review. One Health. 2020;9:100113.
- Shitaye JE, Tsegaye W, Pavlik I. Bovine tuberculosis infection in animal and human populations in Ethiopia: a review. Veterinarni Medicina. 2007;52(8):317-332.
- Data. https://data.worldbank.org/country/ethiopia. Accessed May 14, 2020.
- Romha G, Gebrezgabuher G, Ameni G. Assessment of bovine tuberculosis and its risk factors in cattle and humans, at and around Dilla town, southern Ethiopia. Animal and Veterinary Sciences. 2014;2(4):94-100.
- Tschopp R, Abera B, Sourou S, et al. Bovine tuberculosis and brucellosis prevalence in cattle from selected milk cooperatives in Arsi zone, Oromia region, Ethiopia. BMC Veterinary Research. 2013;9(1):163.
- Vordermeier M, Ameni G, Berg S, et al. The influence of cattle breed on susceptibility to bovine tuberculosis in Ethiopia. Comparative Immunology, Microbiology and Infectious Diseases. 2012;35(3):227-232.
Next story: A Pandemic Urges a Place for Animal Welfarism in the Public Health Sphere
K-State Olathe
22201 W. Innovation Dr.
Olathe, KS 66061-1304
913-541-1220
913-541-1488 fax
olatheinfo@k-state.edu