COVID-19 Pandemic, Present and Future: What Strategies Should We Take?
One Health Newsletter: Volume 12 Issue 2
Authors
Mark Souris
Director of Research
French Research Institute for Development
Jean-Paul Gonzalez
Department of Microbiology & Immunology
Division of Biomedical Graduate Research Organization
School of Medicine, Georgetown University
Faced with the 2019 pandemic of coronavirus disease (COVID-19), there are some burning questions to address about this extraordinary, ongoing phenomenon. First, what strategies are being applied to control the pandemic and what lessons have been learned? Second, how can the world be more prepared and organized to handle such events that are likely to happen again in the future?
Background. Since the 1970s, more than 300 new diseases have emerged. Several species of coronavirus have also emerged. Some species are known to cause mild symptoms (similar to the common cold), while others cause severe disease syndromes, most notably Severe Acute Respiratory Syndrome (SARS) and Middle East respiratory syndrome (MERS). The COVID-19 pandemic creates a multidimensional threat to public health, socioeconomics, and certainly, politics. Despite these recurrences with monitoring systems in place and the extraordinary development of knowledge, humanity still appears to be highly vulnerable to this kind of event.
These astonishing times call for a global consultation of all societal sectors (Fletcher, 2020) to fight against a common threat: the emerging SARS coronavirus 2 (SARS-CoV-2) responsible for COVID-19. This dynamic remains to be mastered as a global health process. Indeed, this global approach is part of the strategies and solutions integrated in the "One Health" concept, and which must ultimately be adjusted according to local resources and the country's population.
Know the threat to fight smarter, not harder. The coronavirus family circulates in domestic and wild animals, subjecting it to continuous genetic variation (Master, 2006). It is rare to see these variants crossing from animal to human. When this event does occur, the variant could display unexpected contagiousness and virulence in humans. For coronaviruses, only three crossing-over events are known beginning with SARS in 2003, MERS in 2013, and SARS-CoV-2 in 2019-2020. SARS-CoV-2 appears to be highly contagious, transmissible from human-to-human, and more virulent than seasonal influenza viruses (Wormser, 2020). SARS-CoV-2 infection occurs in all age groups with severity in the elderly. SARS-CoV-2, like most coronaviruses, induces protective immunity in the short- or medium-term (Zhu, 2004).
What's the best strategy to be prepared and respond? In the absence of a therapeutic solution or a vaccine, what strategy should be adopted to respond, control, and prevent further infection? Between action and inaction (i.e. watching the spread of natural immunity), can enough been done to stop the spread of this disease? If so, how should we begin? While the approach lies in the balance between short-term improvements in human health and the long-term stability of the economy, several strategies should be considered regarding various risks and consequences which are further discussed below:
- Seasonal flu strategy (Smetana, 2018). This method would either allow the disease to circulate freely to achieve herd immunity or allow the virus to naturally dissipate like seasonal flu. The use of seasonal flu vaccine is usually limited to at risk population most of the immunity occurs naturally during the season and after (Hill, 2019). A consequence is the high mortality risk to the elderly or individuals with concurrent health conditions. If applied to the current pandemic, this strategy would be short in duration, lasting for one or two seasons. This strategy would effectively limit the economic consequences of quarantines which is ideal.
- Protecting the weak. Another strategy would be letting the disease circulate as a seasonal flu while actively protecting (e.g. isolation, therapy, vaccine when available) the most vulnerable (when possible), until the disease stops on its own by the lack of transmission. (The vulnerable are protected and the acquisition by others results in mass natural immunity). Most economic activities will be maintained with no confinement of the labor force. However, the cost to protect an extended group of the population will be enormous.
- Protecting the efficiency of the health system. This strategy focuses on letting the disease circulate while slowing the transmission (e.g. isolation, masks, distancing, nursing barrier) as much as possible. The goal would be preventing intensive care units from being overwhelmed while maintaining the essential economic activities. This tactic implies an extended closure of non-essential services and a strong confinement of the remaining population. The economic consequences would be high due to the uncertainty of the pandemic’s duration.
- Stop the epidemic at all costs. The objective would be to completely stop virus transmission as quickly as possible. Extremely strict surveillance and confinement measures would be required as well as ending all non-essential economic activities in regions where transmission is actively occurring. The economic consequences be would significant but is expected to be short in duration. However, international activities, depending on restrictions of other countries in response to COVID-19, could have some bearing on this timeline.
What to expect from these strategies?
The “seasonal flu” strategy would theoretically lead to protective herd immunity before the other enounced strategies. This is a default solution since it would be linked to a high mortality cost, especially in countries with a large population of individuals over 65 years old (Figure 1). The time required to achieve herd immunity would depend mostly on contagiousness, subclinical or asymptomatic carriers, previous immune status of the population, and the efficiency of individual protective measures. However, if the time needed to achieve herd immunity is expected to be short (a few months to a year, depending on the environment), the healthcare system would become overwhelmed, resulting in additional mortality. Therefore, this strategy would be politically difficult to assume given the potentially high number of lives lost.
The “protecting the weak” strategy would theoretically be the best option in the absence of a vaccine or therapy. However, protecting only a part of the population (e.g. based on age or health vulnerability) appears difficult if not impossible with the contagious properties of SARS-CoV-2 virus. In the face of health consequences (e.g. discrimination by age), governments will lean toward limiting such consequences, especially in democratic countries under societal pressure.
The strategy to “protect the health system” is the pragmatic strategy. Considering such an epidemic is difficult to stop and the capacity of the healthcare system is the only parameter accurately known, most democratic middle-to-high income countries would be able to bear the cost of a prolonged economic slowdown. Currently adopted by most of the countries, this strategy is supported by different health systems and sanitary precautions (e.g., quarantine, detection, tracing, intensive care) and carried out under high stress situations relying on the population’s resilience and vulnerability. Ultimately, effective herd immunity will not be achieved while waiting for a hypothetical therapeutic treatment or vaccine solution. If the strategy aims to reduce the disease burden of the epidemic, it may be followed by additional measures to stop the transmission in a second phase (if testing capacity is available to trace all infected persons and their contacts) (Souris & Gonzalez, 2020).
To “stop the transmission” strategy requires strict control of the population (i.e., authoritarian political systems), absolute quarantine compliance, and an expanded tracing of contacts to interrupt the potential chains of transmission.
The two last strategies could potentially trigger regular re-emergences from the reintroduction of the virus from epidemic areas to naïve populations, meaning the same strategy would need to be resumed once again.
Strategy preference based on socioeconomic status
Low- and middle-income countries would favor a “seasonal flu strategy” when the population depends largely on the informal sector (non-essential economic activities), for which the strict cessation of activity would cause unbearable economic losses. These populations appear to be less vulnerable because smaller proportions of the population are elderly when compared to industrialized countries (Figure 1). However, the limited health systems in these countries could result in higher lethality to age groups considered less vulnerable to infection (i.e., individuals 40-65 years old) (Kang & Jung, 2020).
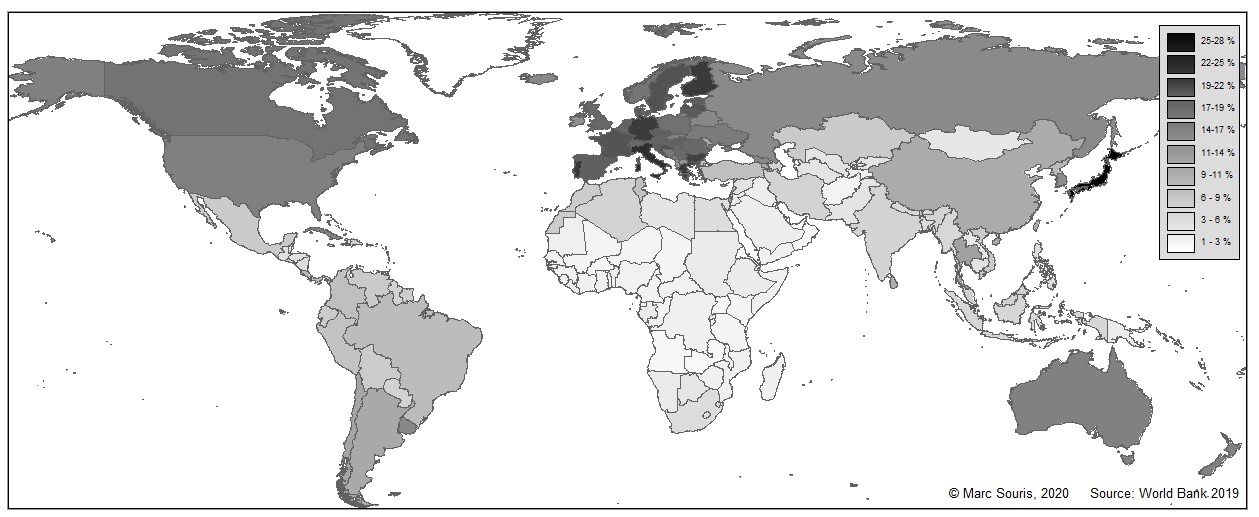
Figure 1: World population of individuals 65 years or older. In 2019, 703 million people were 65 years old or older in the world. (Source: © Steve Barkan and Flat World Knowledge; https://www.peoi.org/Courses/Coursesen/socfwk/ch/ch12d.html).
A ray of hope independent of strategy
Several actions have proven effective in reducing transmission including: testing all suspected cases of virus infection (passive surveillance), followed by isolation of confirmed patients and contact tracing; developing an active surveillance (i.e., virus detection in at-risk populations) use of masks, hygiene, and social distancing. Once developed, rapid tests, therapeutics, and vaccines will certainly complement these strategies (Nussbaumer-Streit, 2020). One positive factor is the still unexplained low incidence observed in several countries like Southeast Asia, Oceania, and Africa, which could be the positive result of pre-existing cross-immunity from another coronavirus to SARS-CoV-2.
Political action. Health has become a primordial and unavoidable injunction of political action, even when an event has a limited impact on overall mortality. In the case of COVID-19, does a collective hallucination of expecting a “zero mortality” as a citizen require sweeping away all other political injunctions? Is this citizen requirement compatible with the level of preparedness of our societies and the related cost and taxes? Many countries acted quickly to follow public health interest first, despite the multiple, incomplete variables given by the life sciences and overlying economic uncertainties. Other countries initially acted with great reluctance (e.g., United States, United Kingdom, Sweden, Mexico, Brazil), but they were drawn to more drastic measures when facing the burden of the disease. Health consequences take priority over economic consequences and financial costs. In short, it is necessary to juggle between “saving” time to address the disease and “wasting” time to address economic recovery. The choice is essentially political.
Conclusion. The world was clearly not prepared for the COVID-19 pandemic. International cooperation at the scientific level was effective and rapid, but international cooperation at the political level was not effective despite the best efforts of the World Health Organization (WHO). All sectors (Buzzell-Saltzman, 2004; Fletcher, 2020) of society now understand that there must be preparation for the next sudden and unexpected emerging pathogen. Not only the health sector is affected, but the political sector as well, both of which must join in a coordinated, anticipatory approach with resources allocated for prevention corresponding to the level of the threat. Ultimately, it is expected that the overall human and financial consequences of such an event will be much higher than the cost of prevention. Facing emerging pandemics, societies must engage in a comprehensive solution aligned with a One World, One Health global policy.
References
Buzzell-Saltzman, L., (2004). The 17 Sectors of sustainable society: How can your town or city become more self-reliant and sustainable? Retrieved August 24, 2020, from http://www.forthefuture.org/assets/articles/col_17_sectors.htm
Fletcher, J. (2020, August 24). What is a social sector? Retrieved August 24, 2020, from https://www.wisegeek.com/what-is-a-social-sector.htm
Hill, E. M., Petrou, S., Lusignan, S. D., Yonova, I., & Keeling, M. J. (2019). Seasonal influenza: Modelling approaches to capture immunity propagation. PLOS Computational Biology, 15(10). doi:10.1371/journal.pcbi.1007096
Kang, S. J. & Jung, S. I. (2020). Age-related morbidity and mortality among patients with COVID-19. Infectious Chemotherapy, 52(2):154-164. doi:10.3947/ic.2020.52.2.154
Masters, P. S. (2006). The molecular biology of coronaviruses. Advance Virus Research, (66), 193-292. doi:10.1016/S0065-3527(06)66005-3
Nussbaumer-Streit, B., Mayr, V., Dobrescu, A. I., Chapman, A., Persad, E., Klerings, I., . . . Gartlehner, G. (2020). Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database of Systematic Reviews, 4(4). doi:10.1002/14651858.cd013574
Smetana, J., Chlibek, R., Shaw, J., Splino, M., & Prymula, R. (2017). Influenza vaccination in the elderly. Human Vaccines & Immunotherapeutics, 14(3), 540-549. doi:10.1080/21645515.2017.1343226
Souris, M., & Gonzalez, J. (2020). COVID-19: Spatial analysis of hospital case-fatality rate in France. MedRxiv. doi:10.1101/2020.05.16.20104026
Wormser, G. P. (2020). COVID-19 versus seasonal influenza 2019–2020: USA. Wiener Klinische Wochenschrift, 132(13-14), 387-389. doi:10.1007/s00508-020-01685-y
Zhu, M. (2004). SARS immunity and vaccination. Cellular Molecular Immunology, 1(3), 193-198.
Next Story: COVID-19: A Typical Emerging Disease: Lessons from Senegal
One Health Newsletter
The One Health Newsletter is a collaborative effort by a diverse group of scientists and health professionals committed to promoting One Health. This newsletter was created to lend support to the One Health Initiative and is dedicated to enhancing the integration of animal, human, and environmental health for the benefit of all by demonstrating One Health in practice.
To submit comments or future article suggestions, please contact any of the editorial board members below.