A Typical Emerging Disease: Lessons From Senegal
Authors
Massamba Sylla, Ph.D.
Medical Entomologist
Vector Control Unit, National Malaria Control Program,
Ministry of Health and Social Action, Dakar, Senegal
Another pandemic. Our planet is facing a pandemic due to a new coronavirus. It emerged in late December 2019, first affecting people who attended the seafood market, followed by healthcare workers who subsequently took care of them, immediately showing its high potential to spread (Li et al., 2020). Chinese scientists sequenced some of the original samples from Wuhan, and the culprit was a coronavirus related to other known coronaviruses that potentially circulates in chiropterans (i.e. bats). It was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This respiratory infection, called coronavirus disease-2019 (COVID-19), quickly reached all of China, spread to Thailand during early January 2020, before spreading to Spain and Europe by January 31, 2020, and the United States. In February 2020, the African continent documented its first COVID-19 case in Egypt and helped further the spread of the disease via worldwide transportation of travelers returning from Asia, Europe, and the United States. The pandemic wave finally covered all continents, except Antarctica, propelled by the unique epidemic characteristic of the virus (low virulence, high infectivity) of the virus from the Atlantic islands on the Indian subcontinent to the Pacific. It is easy to see, in this new disease emergence what roles were played by social, political, and economic agencies, which leads us to reaffirm the importance of a ”One Health“ approach in the prevention and response to such pandemics.
The emerging scenario. The interspecies virus spillover scenario of emergence already documented with Nipah virus and two other coronaviruses—SARS-CoV-1 and the Middle East Respiratory Syndrome (MERS)—is also the case for SARS-CoV-2. All those viruses incubate in bats. Then, after mutation, they spend a transient journey in other animal species including: suids for Nipah virus, civet for SARS-CoV-1, and dromedary for MERS viruses. The viruses mutated again in those intermediate hosts before acquiring the potential to be transmitted to humans by direct animal contact. A dive into the genetics of SARS-CoV-2 concluded this emerging virus might have spent some time infecting both bats and pangolins before it spilled into humans (Duke University Medical Center, 2020). It is essential to note all emerging diseases are related to human actions within the environment and calls for a reconsideration of human-nature interactions.
The spread of the disease. Currently, this vicious SARS-CoV-2 is trying to create problems for African populations. South Africa, Nigeria, Tunisia, and Algeria are already struggling to contain the disease. However, no health system is strong enough to prevent the spread of the disease. Even the most developed countries are powerless to stop the pandemic. To date, all 54 countries of the African continent have COVID-19 cases, yet with relatively low total incidence rates. The SARS-CoV-2 virus does not seem as comfortable in Africa as it does in Europe where 2,017,436 cases were reported as of June 5, 2020 (European Centre for Disease Prevention and Control (ECDPC), 2020). The most afflicted countries are Russia (441,108), United Kingdom (281,661), Spain (240,660), Italy (234,013), and Germany (183,271), with a combined total of 177,828 deaths (ECDPC, 2020). Affected after Europe, the United States became the COVID-19 epicenter by April 11, 2020. By June 5, 2020, John Hopkins School of Tropical Medicine and Hygiene reported 1,872,660 cases, with 108,211 deaths (Johns Hopkins University, 2020). The African continent seems to be relatively spared from large-scale COVID-19 morbidity and mortality rates to date. Africa has reported 169,823 cases, with the five most affected countries being South Africa (40,792), Egypt (29,767), Nigeria (11,516), Algeria (9,831), and Ghana (8,885), for a combined total of 4,743 deaths. Senegal lists 4,155 cases with 45 deaths. Several factors might be in favor of a lower incidence observed in Africa compared to the rest of the globe, including, among others: the potential of pre-existing natural and cross immunity, younger average age of at-risk population, and mass campaigns of chloroquine and ivermectin. However, in Africa most victims of the SARS-CoV-2 suffered from co-morbidities such as diabetes, high blood pressure, and renal failure which are sadly common in the African continent.
|
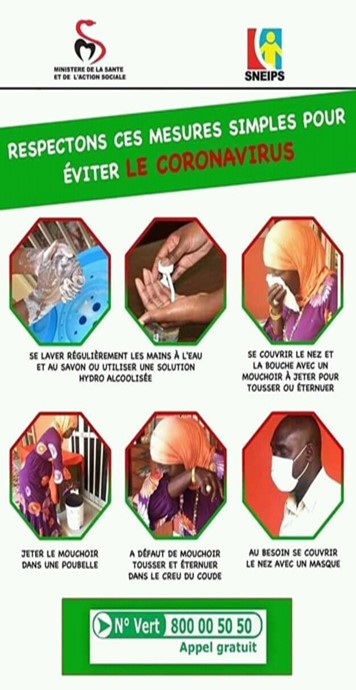
Senegal. Several basic initiatives have been posted and implemented at the national level in Senegal (Figure 1). A state of emergency was declared on March 23, 2020, and a curfew was imposed throughout the country; it is ongoing, though times have been adjusted over the course of the pandemic. The country's health structures have been reorganized and consequently equipped to host any eventually affected patients. People returning from hotspots are recommended to self-quarantine for 14 days. They are then tested to determine if they carry the pathogen and 1) released if their results are negative or 2) moved to a hospital quarantine if positive. Schools and universities are closed, transport is reduced, and strict hygiene rules (hand washes, face coverings, and social distancing) are required in all public spaces and public transportation. The current RNA-based diagnostic done with nose or throat swabs in Senegal is onerous and only targets the presence of viral sequences. The test identifies people with an active infection who are showing the obvious symptoms of COVID-19 like cough, shortness of breath, fever, muscle pain, sore throat, and loss of taste and smell. Serological tests are available which would confirm whether someone has been exposed to the virus, providing useful information for management of the pandemic.
Strategy. The already identified cases of COVID-19 are very sparsely distributed in Senegal and the disease is underdiagnosed. It would be unrealistic to continue the lockdowns and required social distancing for a full year. Fortunately, restriction measures helped contain the virus but were not kept in place long enough to stop secondary transmissions. In May 2020, Senegal decided to re-open markets, churches, mosques, schools, and the weekly mass gathering markets where people from different areas of Senegal and surrounding countries swap goods. Communicable diseases have increased chances for transmission and spread in such densely crowded gatherings. In the absence of serological tests available at the national level, trade, business, and religious activities decided to favor economic activities rather than taking protective epidemiological measures which were a hindrance to business and the traditional economy. The critical measures of a successful response to the propagation of the virus should be early detection and isolation of potentially infectious people. Notably, mass diagnosis is missing in Senegal and most African countries, so suspected cases must fit some current COVID-19 criteria before being screened. This is unfortunate as the SARS-CoV-2 virus has silently found a way to disseminate. However, several responses from the State on lockdown and other transmission barriers in Senegal are emerging. In an interview published in the newspaper L’Observateur (Sylla 2020), it was mentioned that serology would be invaluable for managing the pandemic and predicting its future trend in Senegal (Figure 2).

Figure 2. Cover Page of L'Observateur featuring Massamba Sylla, Dakar, Senegal. (Source: L'Observateur, Num. 4987. Group Futurs Media GFN+M Edit).
Antibody responses to the SARS-CoV-2 will tell whether someone has recently contracted the virus and developed immunity against COVID-19. COVID-19 cases have potentially gone unidentified because asymptomatic individuals are still interacting with susceptible individuals. Four days before showing symptoms, individuals incubating SARS-CoV-2 are potentially transmitting the disease. Early in the outbreak, researchers estimated a SARS-CoV-2 carrier might be able to infect two to three other people on average. Recent studies have argued this number may actually be higher. Undetermined factors seem to underlie the explosive magnitude of COVID-19 in Europe and the United States and its relative morbidity and mortality in Africa. To address a potential immunity of the Senegalese community against COVID-19, a first step will be identifying any possible cross-reacting antibodies which potentially protect against COVID-19, and will ultimately allow Senegal to determine appropriate strategic approaches.
Coronaviridae and the bats of Senegal. Seven new coronaviruses have been discovered in bats in Gabon, but their potential to spill over into people and cause a COVID-19-like pandemic is unclear. Scientists have known coronaviruses can jump from bats to people causing serious illnesses, like the 2002-2003 SARS coronavirus outbreak that was traced back to bats in China. Coronaviruses might have been circulated in Senegal and other parts of Africa, potentially explaining why SARS-CoV-2 is less lethal here. The animal species incriminated in the ongoing pandemic are the bat, Rhinolophus affinis and the pangolin, Manus tricuspis. Sylla et al. (2015) recently published the distribution map of the African counterpart of the SARS-VoV-2 hosts including a bat, Rhinolophus eloquens and the African pangolin (Manis gigantea), both present in Southern Senegal.
Learning from the others. In West Africa, the epidemic transition is well observed. This SARS-CoV-2 was surprisingly new to science; it appeared and quickly extended its sanctuary to new territories among naïve populations that presented a clinical picture never before described. On February 26, 2020, Brazil reported its first case of COVID-19 appearing indifferent to an eventual propagation of the disease. While mayors and governors wanted to implement lockdown measures, the Brazilian President, Jair Messias Bolsonaro, rejected such precautions, increasing the risk for public health by the lack of public awareness, and instead favoring government support of the economy. Today, Brazil is the new epicenter of the COVID-19 outbreak, recording 621,877 cases and 34,212 deaths as of June 5, 2020 (The Brazilian Report 2020). The situation remains of major concern because Brazil is truly vulnerable due to the favelas hosting poor people lacking basic sanitation conditions. As in Sub-Saharan Africa, Latin America has remained one of the last regions of the world to be struck by the pandemic. Located south of equator, Brazilian-black communities of Manaus of the Amazon river are highly affected today. As for the Afrotropical region, there are no distinct genetic features that might support local immunity in Africa, and deny immunity in Brazil, drawing different epidemiological profiles to COVID-19. On January 24, 2020, France recorded its first three cases of COVID-19 in Paris and Bordeaux. The French authorities were confident they could contain any potential epidemic risks as they rely on a public health system apparently efficient. Today, as many other European countries have been impacted as stated above, Africa should capitalize on these lessons.
Back to the fundamentals and how to be prepared. In Africa, most Ebola epidemics were unrecognized because it was confused with other endemic hemorrhagic diseases. Once identified Ebola re-emerged more than 20 times over the past four decades. Emerging and re-emerging zoonotic diseases caused by arboviruses, filoviruses, coronaviruses, paramyxoviruses, or lyssaviruses represent worldwide public health and veterinary concerns. All these emergences are associated with the increasing mobility of the population, pathogen genetic plasticity, and constant changes in landscape/affected ecosystems. Etiological agents of zoonotic viral diseases generally incubate asymptomatically in wild reservoirs then follow different, complex transmission mechanisms before reaching human populations and other permissive animal hosts. Reservoirs and host vertebrates often have vast ranges, which pose an especially enormous challenge to the developing world where their study and related public health programs are often limited.
In order to actively participate within the international concert of prevention through a global health approach, the establishment of an African laboratory network needs to be implemented to improve bio-surveillance programs, preparedness for early warning signs of disease, tackling reemerging diseases, and other health-related events as they spontaneously arise. For the present COVID-19 threat, which is becoming the top health priority in Africa, new and innovative approaches must be implemented to engage all public and private sectors in the fight against this scourge. When facing the threat of the current COVID-19 pandemic (and considering the experiences of many affected countries) a transdisciplinary approach involving scientists, human and social sciences, stakeholders, economists, and policy makers is clearly becoming a priority driven by an effective One Health framework.
References
Duke University Medical Center. (2020). Evolution of pandemic coronavirus outlines path from animals to humans: The virus's ability to change makes it likely that new human coronaviruses will arise. ScienceDaily. https://www.sciencedaily.com/releases/2020/05/200529161221.htm
European Centre for Disease Prevention and Control (ECDPC). (2020). https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases
Johns Hopkins Coronavirus Resource Center. (2020). COVID-19 map. https://coronavirus.jhu.edu/map.html
Li, Q., Guan, X., Wu, P., et al. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med, 382(13), 1199-1207. doi:10.1056/NEJMoa2001316
Sylla, M., Pourrut, X., Diatta, M., Diop, B.M., Ndiaye, M., & Gonzalez, J.P. (2015). Chiropteran and filoviruses in Africa: Unveiling an ancient history. African Journal of Microbiology Research, 9(22), 1446-1472. doi: 10.5897/AJMR2015.7455.
Castro, J.R. (2020) Reopening Stores does not dent e-commerce advances. The Brazilian Report. https://brazilian.report/coronavirus-brazil-live-blog/
Sylla, M. (2020). We're a long way from epidemic peak (in French). L’Observateur, 4987.
One Health Newsletter
The One Health Newsletter is a collaborative effort by a diverse group of scientists and health professionals committed to promoting One Health. This newsletter was created to lend support to the One Health Initiative and is dedicated to enhancing the integration of animal, human, and environmental health for the benefit of all by demonstrating One Health in practice.
To submit comments or future article suggestions, please contact any of the editorial board members below.